

Case report
Regarding a case of arteriovenous malformations of the left parietal lobe
A propósito de un caso de malformaciones arteriovenosas del lóbulo parietal izquierdo
Rolando Dornes-Ramón1 https://orcid.org/0000-0003-4365-5237
https://orcid.org/0000-0003-4365-5237
Yander Luis Izaguirre-Campillo2* https://orcid.org/0000-0001-7669-5951
https://orcid.org/0000-0001-7669-5951
Lizandra Pujol-Arias3 https://orcid.org/0000-0003-2652-6513
https://orcid.org/0000-0003-2652-6513
1Master of Science in Infectious Diseases. First and Second Degree Specialist in Imaging. First Degree Specialist in Integrative General Medicine. Auxiliar Professor. Junior Research Fellow. Hamad Medical Corporation. Hamad General Hospital. Doha, Qatar.
2Cardiology Resident Physician. Scientific Category: Research Trainee. “Hermanos Ameijeiras” Clinical-Surgical Hospital. Havana, Cuba.
3Havana University of Medical Sciences. Sixth-Year Medical Student. “Calixto García” Faculty of Medical Sciences. "Calixto García" University Hospital. Havana, Cuba.
* Corresponding author. Email:  yanderizaguirrecampillo@gmail.com
yanderizaguirrecampillo@gmail.com
ABSTRACT
Introduction: arteriovenous malformations are a rare disease of the central nervous system that occurs as a result of a fistulous connection between arteries and veins without intervention of the preexisting capillary bed. Its incidence is approximately 1.34 per 100,000 inhabitants in developed countries. It primarily affects men and the areas corresponding to the anterior, middle, and posterior cerebral arteries.
Objective: to describe a case of atypically located cerebral arteriovenous malformations in adults.
Case presentation: a case with varied characteristics was presented in which an arteriovenous malformation located in the left parietal lobe of the cerebral cortex was diagnosed by neuroimaging. In this patient, early medical intervention prevented the development of cerebral hemorrhage. She was successfully treated with Ganma Knife radiosurgery and progressed well without recurrence during follow-up.
Conclusions: the diagnosis of this condition is made using neuroimaging techniques in all patients with these symptoms. Ganma Knife radiosurgery may be the ideal therapy in some cases, but not in others; it all depends on how the patient is classified according to the Spetzler and Martin scale. This article provides solid evidence on the role of imaging in the diagnosis and preoperative stratification of these patients.
Keywords: case reports; intracranial arteriovenous malformations; neuroimaging; parietal lobe; radiosurgery.
RESUMEN
Introducción: las malformaciones arteriovenosas constituyen una enfermedad poco común del sistema nervioso central que ocurre a consecuencia de una conexión fistulosa entre arterias y venas sin la intervención del lecho capilar preexistente. Su incidencia aproximada es de 1,34 por cada 100 000 habitantes en países desarrollados. Afecta fundamentalmente al sexo masculino y las zonas correspondientes a las arterias cerebral anterior, media y posterior.
Objetivo: describir un caso de malformaciones arteriovenosas cerebrales de localización atípica en el adulto.
Presentación del caso: se presentó un caso de características variadas en el que se diagnosticó, mediante neuroimagen, una malformación arteriovenosa localizada en el lóbulo parietal izquierdo de la corteza cerebral. En esta paciente la actuación médica temprana permitió que no se desarrollara la forma de hemorragia cerebral. Se trató exitosamente con radiocirugía Ganma Knife y evolucionó de forma adecuada sin recidivas durante su seguimiento.
Conclusiones: el diagnóstico de esta afección se realiza mediante técnicas de neuroimagen en todo paciente con esta sintomatología. La radiocirugía con Ganma Knife puede ser la terapia ideal en algunos casos, no así en otros, todo dependerá de cómo sea clasificado por la escala de Spetzler y Martin. Este artículo aporta evidencia sólida sobre el papel de la imagenología en el diagnóstico y estratificación preoperatoria de este tipo de pacientes.
Palabras clave: informes de casos; lóbulo parietal; malformaciones arteriovenosas intracraneales; neuroimagen; radiocirugia.
Received: 2025/07/13
Approved: 2025/08/18
Cerebral arteriovenous malformations (AVMs) are vascular abnormalities characterized by a direct fistulous connection between arteries and veins, bypassing the normal capillary bed. They represent a group of uncommon anomalies of the central nervous system with variable locations; they are defined by an arteriovenous shunt, where one or more arterial pedicles supply a vascular nidus, resulting in early drainage into an outflow venous channel.(1-3)
They are primarily located in the area of the major cerebral arteries (anterior, middle, and posterior), but they can occur in other areas and receive supply from various main arterial trunks and the leptomeningeal arteries. Their forms are diverse; the most common is a wedge shape, with input from one or several cortical arteries, followed by the nidus of abnormal vessels and drainage into the superficial and deep veins.(1)
The prevalence of arteriovenous malformations in the general population is 10 to 18 per 100,000 adults. Their forms of presentation can be: hemorrhagic (58 %), convulsive (34 %), or neurological focal (8 %). Hemorrhages are associated with a 5-30 % mortality rate worldwide.(4) Cerebral arteriovenous malformations account for 15 % of all arteriovenous malformations; there is one new case per 100,000 people per year worldwide, and they are responsible for 1-8 % of strokes, with a slight male predominance. In the United States, an annual incidence of 1.34 per 100,000 people is reported.(5) The most frequent mode of presentation is intracranial or subarachnoid hemorrhage, which accounts for 50 % of adult cases and up to 4 % in children. Between 15 % and 20 % result in fatal outcomes.(6)
The true prevalence of cerebral arteriovenous malformations in any population is difficult to estimate. There are no known epidemiological studies on the incidence of this condition in Cuba. For this reason, it was decided to present this article with the objective of describing the case of a patient diagnosed with cerebral arteriovenous malformations in an atypical location, based on what is referenced in the literature on the subject.
A 47-year-old white female patient, with no relevant personal history, from a rural background, works as a preschool educator. Her mother has a history of hypertension for approximately 55 years. She reports drinking coffee in the mornings as a habit. Five years ago, she began experiencing episodes of transient right-side hemibody paralysis, which resolved spontaneously after several hours and occurred with a frequency of about four times per year. She also presented with vomiting preceded by nausea (up to four times per day), which was copious and bilious in content. A year and a half ago, she suffered a generalized seizure, which recurred three months later. The frequency of these seizures increased to one or two per month. She is currently on a treatment of 200 mg of carbamazepine every six hours, which has reduced the frequency of the seizures to approximately one every three months.
One month ago, she began experiencing an intense, stabbing occipital headache, which rarely radiated to the left parietal area. It appeared and resolved spontaneously and was accompanied by dizziness and numbness of the tongue. Three days ago, she developed paralysis of the right side of her body and rapidly progressing ipsilateral numbness, which prompted her to seek medical care. She was admitted to Hamad General Hospital in the Qatari city of Doha for further diagnosis and the implementation of therapeutic measures.
The institution's Research Ethics Committee approved the publication of the case report. Informed consent was previously obtained from the patient for undergoing therapeutic procedures and for the disclosure of her case for scientific purposes, without sharing contact information of the patient or family members, or any personal data.
The initial laboratory workup was carried out with the following results: hemoglobin: 13.7 g/dL (RR: 12-14 g/dL); hematocrit: 0.41 % (RR: 0.37-0.47 %); leukocytes: 6.3 x 10⁹/L (RR: 5-9 x 10⁹/L); platelets: 452 x 10⁹/L (RR: 150-350 x 10⁹/L); glycemia: 5.0 mmol/L (RR: 3.85-5.55 mmol/L); creatinine: 67 mmol/L (RR: 44.2-132.6 mmol/L); erythrocyte sedimentation rate: 113 mm/h (RR: <20 mm/h); albumin: 26 g/L (RR: 32-45 g/L); cholesterol: 4.1 mmol/L (RR: 3.87-6.50 mmol/L); triglycerides: 2.34 mmol/L (RR: 0.35-1.70 mmol/L); and globulins: 20 g/L (RR: 28-35 g/L).
A non-contrast and subsequent intravenous contrast-enhanced axial computed tomography scan of the head was carried out. It revealed a hyperdense, rounded lesion with a whorled appearance and a density of 54 HU, located in the left parietal lobe (Figure 1 a, b, c). A CT angiography of the head showed a hyperdense (54 HU), rounded, whorled-appearing lesion located in the left parietal lobe within the territory of the middle cerebral artery, with drainage into the inferior sagittal sinus (Figure 2).
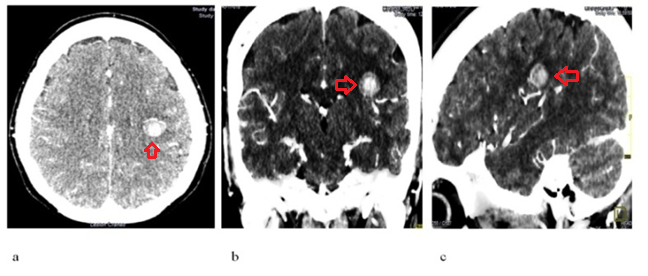
Fig. 1 - CT scan of the head without and with contrast: a (axial view), b (coronal view), c (sagittal view). The previously described rounded, white (hyperdense) image is indicated with a red arrow.
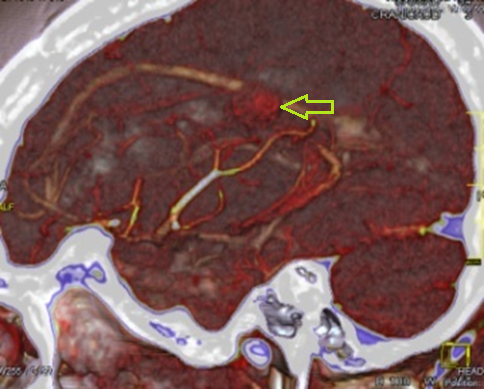
Fig. 2 - CT angiography of the head, sagittal sequence, showing the arteriovenous nidus as a rounded image indicated by a yellow arrow.
Taking into account the findings from the imaging studies, a cerebral arteriovenous malformation was diagnosed. A nuclear magnetic resonance imaging was decided upon to obtain more specific measurements prior to the surgical procedure. An arteriovenous nidus volume of 25 cm³ was confirmed, along with peripheral neoangiogenesis and multiple subpial fistulas. Based on the provided imaging data, it was assigned two points (Class II, low surgical risk) on the Spetzler-Martin scale(7) (one point for a size smaller than 3 cm in linear diameter and one point for involving eloquent sites).
In accordance with the diagnosis and Spetzler-Martin (7) classification, which indicated a low surgical risk, the patient was referred to the neurosurgery department at Hamad General Hospital, where she underwent radiosurgery. The therapeutic procedure was successfully carried out without major complications. The patient experienced improvement in all the symptoms that had led to her admission. Over the past year, she has maintained a stable course with no associated complications.
Arteriovenous malformations are highly unusual conditions that can occur anywhere in the central nervous system, with variable frequency depending on their characteristics. Typically, this type of abnormality manifests more frequently in males and, according to López-Flores et al.,(8) based on clinical observation and the theory of cerebral lateralization development, they more commonly affect the left cerebral hemisphere.
It is known that arteriovenous malformations present a wide variety of symptoms; the hemorrhagic form is the most common, with a prevalence of approximately 46–59%, and is also the most lethal among them.(1,8,9) However, it is not the only one; other notable varieties include chronic headache, convulsive forms, progressive mental deficiency, heart failure, and hydrocephalus (in pediatric ages).(1,8)
In the presented patient, the disease progressed to the chronic headache and convulsive forms; she eventually developed paralysis and progressive numbness. The latter was the most pronounced symptom. However, it was noteworthy that the hemorrhagic variant did not occur, as demonstrated by radiographic studies.
Most arteriovenous malformations do not become symptomatic until the third decade of life. Studies show that up to 80 % become symptomatic after the age of 15, most frequently near or beyond the age of 30. This can be explained by pathophysiological mechanisms whereby, as the condition develops over time, the afferent arteries achieve greater dilation, acquire areas of focal hyperplasia, and occasionally develop aneurysms.(8,10) In this context, a 47-year-old patient was analyzed, which aligns with what is reported in the international literature.
The presumptive diagnosis was made based on clinical elements, as well as the use of computed axial tomography; it was corroborated by performing cerebral panangiography, magnetic resonance imaging, and CT angiography. A non-contrast computed tomography scan is a low-sensitivity study for these lesions; however, this ancillary test can raise suspicion of the lesion when other findings are observed, such as calcifications, spontaneously hyperdense, rounded, or serpentine images, or the presence of intraparenchymal remnant malformation areas with zones of higher density within them, exactly as evidenced in this case. Therefore, computed tomography and magnetic resonance imaging are considered the most commonly used techniques in this type of diagnosis.(11)
Superselective angiography can be another diagnostic tool for these conditions; this ancillary study provides relevant hemodynamic and physiological details for decision-making.(12) In this case, other studies were not employed because a precise diagnosis was established without difficulty, as well as the differential diagnosis with clinically similar conditions such as: intracranial tumors, cerebral hemorrhages, central nervous system infections, or neurotoxin use. Currently, in the presence of an arteriovenous malformation, the Spetzler-Martin scale(7) published in 1986 is used, regardless of the modifications it has undergone over the years or the controversial opinions of some authors.(7,13)
Among the therapeutic options considered, the first is expectant management, followed by symptomatic medical treatment (example, anticonvulsant therapy), surgical resection, endovascular therapy, or stereotactic radiosurgery, not to mention the possibility of combining any of these. There are also factors that influence decision-making, such as: age, underlying diseases, presence or absence of hemorrhagic manifestations, location and extent of the malformed area, as well as the presence or absence of aneurysms within the nidus.(1)
Brauner et al.(14) concluded that the combination of maximum endovascular embolization and complete surgical resection in a single session for this type of patient resulted in a high cure rate and low morbidity and mortality. For the treatment of this patient, after extensive evaluation, Gamma Knife radiosurgery was chosen, which allowed for the slow, progressive removal of the malformed area within a one-year period, without major complications. Although in most reported cases the disease manifests clinically near the third decade of life, it can also begin earlier or later, as observed in this patient, suggesting that a broader age range should be considered for diagnosis.
Taking into account the observations in this case and preceding studies, it can be proposed that in a patient between 15 and 50 years of age presenting with seizures, headaches, sensory-motor disturbances, with or without associated hemorrhages, an arteriovenous malformation should be suspected. This must be corroborated using radiological studies, particularly cerebral angiography, to classify it according to the Spetzler-Martin scale(7) and to select an appropriate and individualized therapeutic approach for each case.
The main limitation of this study was the short postoperative follow-up period, which did not allow for inference of long-term outcomes or observation of possible recurrences of this disease.
The clinical presentation plays a fundamental role in the presumptive diagnosis of arteriovenous malformations; however, neuroimaging studies are required for confirmation, as these abnormalities are considered a type of medical emergency. Once the disease is diagnosed, the neurosurgeon and interventional radiologists must choose the most appropriate therapy for the patient after analyzing each specific case, depending on the location, extent, and neurological involvement. Radiosurgery with Gamma Knife is a good example of the therapeutic measures that can be used for this condition. This article provides clinical evidence in the diagnosis of a complex cerebrovascular disease and reflects how imaging plays a crucial role in identifying the abnormality, as well as in its stratification to allow for the most reliable treatment.
1. García-Leonard JI, Sánchez-Lozano A, Valladares-Valle M. Intraparenchymal Hematoma as the Beginning of an Arteriovenous Malformation. Case Report. Rev Finlay [Internet]. 2020 [cited 2025 Jun 15];10(4):445-51. Available from: http://scielo.sld.cu/pdf/rf/v10n4/2221-2434-rf-10-04-445.pdf
2. Fiallos-Brito EJ, Villacrés-Gavilanes SC. Brain arteriovenous malformation. Case report. Rev inf cient [Internet]. 2024 [cited 2025 Jun 15];103:e4465. Available from: https://revinfcientifica.sld.cu/index.php/ric/article/view/4465/6240
3. Nicolás-Cruz CF, Mondragón-Soto MG, Aguilar-Calderón JR, Melo-Guzmán G. Bimodal management of aneurysms associated with cerebral arteriovenous malformations. Case report and brief review of the literature. Cir cir [Internet]. 2020 [cited 2025 Jun 15];88(Suppl 2):79-83. Available from: https://www.scielo.org.mx/pdf/cicr/v88s2/0009-7411-cir-88-S2-79.pdf
4. Goland J. Malformaciones arteriovenosas cerebrales incidentales grado 1, 2, 3 en mi consultorio. Rev Argent Neuroc [Internet]. 2022 [cited 2025 Jun 15];36(4):1-4. Available from: https://www.ranc.com.ar/index.php/revista/article/download/466/631
5. Bokhari MR, Bokhari RA. Arteriovenous Malformation of the Brain [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 [cited 2025 Jun 15]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430744/
6. Cordero-Campos A, Espíritu N, Ramírez-Espinosa A, Yaipen-Chancafe S, Medina-Bendezú D. Clinical–epidemiological characteristics and management of cerebral arteriovenous malformations at the Neurosurgery Service of the Instituto Nacional de Salud del Niño San Borja, 2015–2017. Horiz Med [Internet]. 2021 [cited 2025 Jun 15];21(2):e1332. Available from: http://www.scielo.org.pe/pdf/hm/v21n2/1727-558X-hm-21-02-e1332.pdf
7. Spetzler RF, Martin NA. A proposed grading system for arteriovenous malformations. J Neurosurg 1986;65:476-83.
8. López-Flores G, Fernández-Melo R, Cruz-García O. Etiopathogenesis and physiopathology of cerebral arteriovenous malformations. Arch Neurocien [Internet]. 2010 [cited 2025 Jun 15];15(4):252-59. Available from: https://www.medigraphic.com/pdfs/arcneu/ane-2010/ane104h.pdf
9. Miron I, Prună VM, Visarion DM, Petrescu GED, Gorgan RM. Natural History and Predictors for Hemorrhage in Supratentorial Brain Arteriovenous Malformations. J clin med [Internet]. 2024 [cited 2025 Jun 15];13(13):3760. Available from: https://www.mdpi.com/2077-0383/13/13/3760
10. Requejo F, Mengide JP, González-Dutra ML, Mantese B, Lipsich J. High-flow vascular malformations of the brain in pediatrics: Experience in a tertiary care children’s hospital. Arch Argent Pediat [Internet]. 2021 [cited 2025 Jun 15];119(3):152-61. Available from: https://sap.org.ar/docs/publicaciones/archivosarg/2021/v119n3a04.pdf
11. González-Matos JC, Dos Santos-Poleo Y, Pérez-Sánchez LI, Álvarez De Eulate-Garcia MT, Montesinos O, Barjau JJ, et al. Manejo diagnóstico no intervencionista de las malformaciones vasculares cerebrales. seram [Internet]. 2022 [cited 2025 Jun 15];1(1):[about 13 p.]. Available from: https://piper.espacio-seram.com/index.php/seram/article/view/9409/7875
12. Kocur D, Przybytko N, Hofman M, Jamróz T, Ignatowicz A, Baron J, et al. Endovascular treatment of small cerebral arteriovenous malformations as a primary therapy. Pol J Radiol [Internet]. 2018 [cited 2025 Jun 15];83(1):e143-50. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC6047079/pdf/PJR-83-32749.pdf
13. Nesbit GM. Neurovascular disease and syndromes: Diagnosis and therapy in children. Handbook Clin Neurol [Internet]. 2021 [cited 2025 Jun 15];176(3):305-23. Available from: https://www.sciencedirect.com/science/article/abs/pii/B9780444640345000158
14. Brauner R, Smajda S, Chauvet D, Aldea S, Escalard S, Désilles JP, et al. Curative Treatment of Brain Arteriovenous Malformations Combining Endovascular and Surgical Approaches Consecutively. World neurosurg [Internet]. 2025 [cited 2025 Jun 15];197:123896. Available from: https://www.sciencedirect.com/science/article/pii/S1878875025002529/pdfft?md5=541f764fa148858767f23416a14d3c51&pid=1-s2.0-S1878875025002529-main.pdf
Conflict of interest
The authors declare no conflicts of interest.
Author's contributions
Rolando Dornes-Ramón: conceptualization, data curation, methodology, project administration, resources, software, supervision, validation, visualization, writing, review, and editing.
Yander Luis Izaguirre-Campillo: formal analysis, investigation, methodology, project administration, software, validation, visualization, writing - original draft.
Lizandra Pujol-Arias: investigation, methodology, resources, validation, visualization, and writing - original draft.
Funding
Hamad Medical Corporation. Hamad General Hospital. Doha, Qatar.
 Esta obra está bajo una licencia internacional Creative Commons Attribution4.0/International/Deed
Esta obra está bajo una licencia internacional Creative Commons Attribution4.0/International/Deed